I wanted to start this article with an opening like “Every country has problems”; which later turned into “The medical education sector is sickening and I am hurt” or “The noble profession and its education is tarnished”. But as I kept researching about NEET, my opening lines kept changing. In fact, one point I was like blame the UPA for this (yes they are to blamed and you will see the write up they can be blamed for about say 90% of nation’s problem); but we are product of our own government. However, in the end, it all boiled down to lack of political will (historically) and secondly, a need to overhaul an entire system. Pinning down on one thing or two things is difficult.
We started this article focusing on the issue on NEET at hand; but realized on a root cause study there are far too many moving parts which have snowballed into this crisis. Accordingly, with an intent of providing a holistic perspective, we decided to focus not only on NEET but also other issues impacting the Medical Education sector. Accordingly, the article focusses on:
- Legal and related issues faced by NEET since inception
- Current entrance test system and expected impact of NEET
- Observation of Parliamentary Standing Committee (PSC) on MCI (Medical Council of India)
- Structural changes required
We leave the reader to draw conclusion based on the facts at hand and also advise them to read the PSC report (link in the bottom) for further insights.
The point we wish to drive here is that the NEET or having a Unified Common Entrance is one of the steps (structurally important) in correcting a huge malaise that has plagued the medical education system. In fact, we wish to point to our readers and political personnel at helm at this is really a BABY step in comparison to the issues with the governing council. Yes, it’s a step in right direction but a lot needs to be done.
BRIEF HISTORY OF NEET
The NEET exam notified by the Medical Council of India is a unified exam for admission for MBBS or Post Graduate course. The NEET exam enabled the students to select any college in the country, making it a central examination just like an entrance test for IIT or NIT. 24th May 2016 should be marked as an important day for medical aspirants here onwards. The National Entrance cum Eligibility Test (NEET) received a Presidential assent, which foreshadows Supreme Court’s May 9 judgement allowing states to conduct their own entrance exams for this academic session.
Timeline of NEET
NEET was held once in 2013; and was introduced in the UPA Era. In fact, early seeds for the examination were highlighted during the Hon ex-PM Manmohan Singh’s 2010 Independence Day speech. However, the issue was later put on back-burner and went through multiple legal and political speed-breakers; to the extent been closeted in 2013; after the first entrance test.
Advocate Karan Seth (representing GOI) on the NEET issue at Supreme Court highlights following merits of NEET:
- Reduction in mental and financial burden on medical aspirants appearing for multiple entrance examinations
- Prevention of malpractices such as donations, and fees camouflaged as donations
- Emphasis on merit as the only criteria for admission
The following table gives a bird’s eye view of the NEET issue.
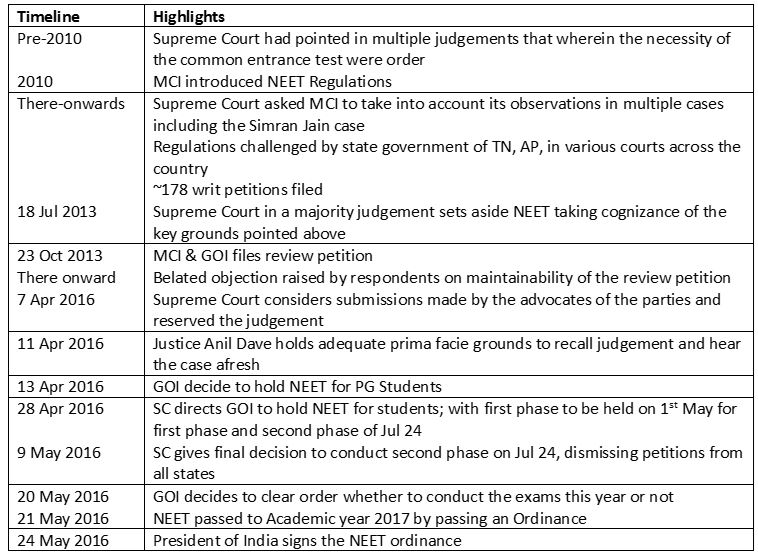
Source & Notes:
Excerpts from an article written by Advocate Karan Seth (appearing on behalf of Indian Government) for the NEET
http://mirrorreport.com/net-exam-complete-timeline-2010-2016/4499/
Despite the above merits pointed out, close to 178 petitions challenged NEET on the following grounds:
- The triple test laid down in the PA Inamdar case that the admission procedure must be fair, transparent and non exploitative was being followed by institutions and there was no violation.
- MCI has no power to conduct examinations.
- NEET is violative of the rights of private medical colleges under Article 19(1)(g), that is, freedom to practice any profession, or to carry on any occupation, trade or business
- NEET violates the rights of religious and linguistic minorities to establish and administer educational institutions as guaranteed under Article 30 of the Constitution.
- Regulations, flowing from a power given under a statute, cannot have an overriding effect over the fundamental right guaranteed under Articles 25, 26, 29(1) and 30 which protect religious practices and the rights of minorities to establish and administer educational institutions.
- Furnishing of regulations to the state government for consideration under Section 19A(2) of the Indian Medical Council Act (IMC ACT) was mandatory and had not been done. Section 19A(2) essentially states that all regulations that the MCI wants to notify must be first sent to the State Government to provide their opinion.
The whole NEET issue was challenged in media given that it’s unfair to students and about 6.5 Lakh student were to suffer. Yes, this issue is true and many students had given the state medical entrance exams; and I believe the stance taken by the government to partially postpone the NEET implementation via Ordinance is fair. We will honestly not delve into this topic of student being impacted as it is adequately covered on various media outlets.
The important point that has come is that NEET is applicable to private educational institutes”. This is the biggest Game Changers. This has such far reaching ramifications, that it will change the way Medical Institutions operate in this country; as explained in the ensuing section.
INTO THE CURRENT SYSTEM OR WHAT HAS BEEN THE LEGACY?
Currently, medical aspirants have to give about 3 exams to get their colleges. For example, the students in the State of Maharashtra are subjected to following exams:
- MH-CET for state government colleges,
- An association exam for the private medical colleges and
- Central exam (AIPMT) for admissions in national level colleges.
In fact, some students can give intra-state examinations, if they prove their lineal descendants are from those states. In fact, one of my cousin (from MH) was planning to give an exam in Karnataka, however, since we are all Maharashtrians and none of our descendants are even out of Pune, hence it was not possible.
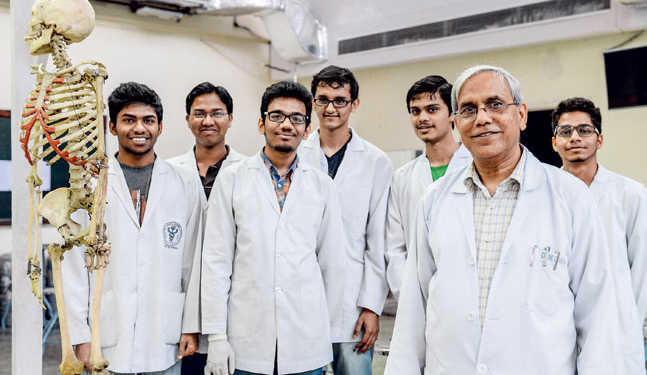
Honestly, I was flabbergasted that there is such a wrong system for the admissions in the most critical education system in India. For this article, I was fortunate that some of my cousins are either doctors or some are undergoing examinations, which led me to meet some of their professors (from Government colleges) to get further insights. What was great to hear was that, everyone was highly in favor of NEET and were praying it gets approved and becomes functional at the earliest. The private medical colleges have made a business of the noble profession. In fact, anecdotally, I am told that none of the merit students vie for Private Medical colleges; primarily because most of the students studying there are paying high donations and in the college is den of sub-standard education. The quality of education in Government colleges and the exposure in the affiliated Government hospitals is far too high vis-à-vis the Private colleges. With this insight from some professors and students; the other insight I had received earlier was from a particular private medical college administration, wherein they had bookings (mind you BOOKINGS) for MBBS for next two years. In fact, the kind of statistics that get published about the donations in the private medical colleges are not far from truth; but I would say are rather understated. The concluding portion of the write up shall give further insights.
GALLERY VIEW OF THE CORRUPTION LACED ADMISSIONS
Times of India ran an article that the market for black money on medical colleges is to the tune of Rs. 12,000 cr. The article further states that ‘Of the 422 medical colleges in India, 224 are private, accounting for 53% of MBBS seats. Many of these colleges are running with little or no facilities, no patients and fake faculty. The going price for an MBBS seat could range from Rs. 1 crore in colleges in Bangalore to Rs 25-35 lakh in some in UP. Seats in MD in radiology and dermatology cost up to Rs 3 crore.’ The article points that the PG seat are been offered at Rs. 3.0 cr., for radiology, ortho and dermatology streams. In fact, of the total value of ‘Seat Sale’ is about Rs. 9000 cr., just from the MBBS stream. Add to those statistics, most of the private colleges with management quota and NRI quota have a seat sale to the extent of 60% of total seats. This is quite alarming and incomprehensible.
DEEP INSIGHT INTO THE SYSTEM THAT HAS FOSTERED THIS CULTURE
Medical Council of India and Dental Council of India regulates the quality of medical education and awarding the affiliation to colleges. This is based on the regulations prescribed as standards for accreditation and they are quite detailed to the extent of student teacher ratio, requirement of patients for the teaching hospital, among others. However, these regulations are criticized at been unrealistic and focusing only on infrastructure; without merit to quality of teaching or even having a methodology to judge quality of teaching.
In Feb 2012 edition of ‘Indian Medical Res Journal’, there was detailed article titled “Medical Seats being Sold!”; which pointed out to some interesting points regarding the corruption in the Medical Colleges and related to MCI. An important case was of MCI President Ketan Desai who was arrested on charges of corruption, which led to dissolution of MCI in 2010. This was despite the fact that Desai was already booked for corruption 2001; although he managed to regain his president-ship in 2009. In 2010, Desai and three others were caught for corruption for recognition of private medical college. In fact, the article pointed that this re-recognition of MCI further gave rise for a more corrupt practices and was also responsible for such stanch stand by the Private Medical colleges. The point is from 2010 and in fact before that everyone seems quite aware of the corrupt practices at work at MCI and private colleges. (Annexure to the write-up in end shows the statistics of Private Medical colleges vs. Government colleges)
We feel, the seeds of the corruption or let’s say an unhindered autonomy to MCI arises from two core constitutional issues. The provision of Health care part of State List while the medical education is part of Concurrent list. So, providing say a gross budgetary support for this education and maintaining standards become part of the Centre’s responsibility while providing service becomes a State responsibility. Moreover, the medical education part of Concurrent list, it is more of State prerogative than Centre’s issue. This part responsibility on one end and part of other end leads to confusion, creation of lobbies, and issues of continuous legal representations (which were evident on the problems face by Governments on changing the MCI Act).
PARLIAMENTARY COMMITTEE REPORT ON MEDICAL COUNCIL OF INDIA
The Parliamentary Standing Committee (PSC) on Health and Family Welfare presented its Ninety Second report on the Committee and Functioning of the Medical Council Of India. The previous PSC had recognized Medical Council of India as a matter of study. During the course period from 25th Sep 2014 to 1st Mar 2016, the PSC held multiple meetings and including visits to Medical Colleges, interviews with MCI officials, among others. The Standing Committee on Health and Family Welfare (Chair: Mr. Ram Gopal Yadav) submitted its report on the Medical Council of India (MCI) on March 8, 2016.
The Ministry of Health informed the Parliamentary Standing Committee that as per MCI records there are 9.29 lakh doctors registered in the Indian Medical Register as on 31.03.2014. Assuming 80% availability, it is estimated that ~7.4 lakh doctors may be actually available for active service. It gives a doctor population ratio of 1:1674 against the WHO norm of 1:1000. At present, every year around 55,000 doctors and 25,000 PG doctors are passing out from various colleges. At this rate of growth, the country should have a doctor (allopathic)-population ratio of 1:1250 for a population of 133 crores by 2020 and 1:1075 by 2022 (population: 136 cores). However, the Committee has been informed by an expert who deposed before the Committee that doctors cannot be produced overnight and if we add 100 medical colleges every year for the next five years, only by the year 2029, will the country have adequate number of doctors. As of 2010-11, India has only 6.5 doctors per 10,000 of population, as compared to 17.6 in Brazil, 14.6 in China, 27.7 in UK, and 24.2 in USA. This is far short of the global average and even below the target of 1 for 1000 of population recommended by the High Level Expert Group Report on Universal Health Coverage for India.
Brief about the MCI
The Ministry of Health and Family Welfare in the background note submitted to the Committee stated that the Medical Council of India was established in 1934 under the Indian Medical Council Act, 1933, with the main function of establishing uniform standards of higher qualifications in medicine and recognition of medical qualifications in India and abroad. The Act was repealed and replaced by a new Act in 1956. The Indian Medical Council Act, 1956 was further amended in 1964, 1993, 2001.
In fact, in 2010 during the Independence Day the Hon’ PM of India, Mr. Manmohan Singh mentioned about two separate councils for higher education and health respectively. However, the project dropped as the PM later stated, when matter was presented to him, that further public consultation is needed. However, as pointed out above despite the 2010 arrest MCI President. During 2010 to 2013 there were multiple attempts made to amend the MCI Act, which would provide for better governance.
Key observations and recommendations of the Committee include:
Observations
The PSC observed that MCI as a regulator of medical education has repeatedly failed on all its mandates over decades. Some of the key stark observations against the MCI are as under:
- failure to create a curriculum that produces doctors suited to working in Indian context especially in the rural health services and poor urban areas; this has created a disconnect between medical education system and health system
- failure to maintain uniform standards of medical education, both undergraduate and post-graduate
- devaluation of merit in admission, particularly in private medical institutions due to prevalence of capitation fees, which make medical education available only to the rich and not necessarily to the most deserving
- little oversight of PG medical education leading to huge variations in standards
- abysmal doctor population ratio
- failure to create a transparent system of medical college inspections and grant of recognition or de-recognition
- failure to oversee and guide the Continuing Medical Education in the country, leaving this important task in the hands of the commercial private industry
The important point raised by the report on Page 90 point 13.2 states that; its not just the MCI that is to be blamed but successive Governments share the burden of failure of Medical education system. The failure is not just the Central but also the State government. Since, the need to evolve the act has been underway for multiple years (since 2011), the PSC notes “Rather than seizing the opportunity to come up with a better Bill, the Ministry remained apathetic to the state of affairs and did not respond with vigorous corrective measures.” In fact, “Nowhere in the world is there an educational process oversight, especially, of medical education done by an elected body of the kind that MCI is”.
Keeping all these facts in mind, the Committee is convinced that the much needed reforms will have to be led by the Central Government. The MCI can no longer be entrusted with that responsibility in view of its massive failures. The people of India will not be well-served by letting the modus-operandi of MCI continue unaltered to the detriment of medical education and decay of health system.
Recommendations
Composition: MCI is largely an elected body and contains only medical doctors. In light of issues arising due to the its elected nature (disproportionate private representation, etc.), the Committee recommended that a regulatory framework must be set up under which regulators are appointed through an independent selection process.
Establishment of colleges: The Committee observed that the present requirements for establishing a medical college are based only on physical space, infrastructure and rigid faculty requirement. The land requirement leads to high initial investment due to which the government and genuine parties (interested in providing medical education) cannot open colleges. The existing minimum standards are causing impediments in the establishment and expansion of medical colleges. It recommended that the requirements for physical infrastructure must be reduced accordingly.
Medical education: As the two stages of medical education (undergraduate and postgraduate) require different kinds of expertise, they should be regulated separately (through setting up of separate boards). Further, the Committee recommended that in order to tackle the issue of high capitation fees and to bring transparency, etc., the central government must introduce a common entrance exam for undergraduate, postgraduate and super specialty courses. To standardise the competencies etc. of graduating doctors, an exit test must be introduced for under and postgraduates.
Accreditation: The Committee observed that the functioning of the MCI leads to conflict of interest as it gives permission to establish medical colleges and also ensures quality of education. Therefore, an independent and autonomous accreditation body must be set up which will be responsible for ensuring the quality of education.
Professional conduct: The Committee observed that the present focus of the MCI is only on licensing of medical colleges. There is no emphasis given to the regulation of medical ethics. In light of this, the Committee recommended that the areas of medical education and medical practice should be separated. A separate board of medical ethics should be set up which will be responsible for developing mechanisms for the promotion of medical ethics. Further, the government must establish a system of auditing medical practice.
Indian Medical Register: According to the Ministry the doctor-population ratio in India is 1:1674 as against the WHO norm of 1:1000. The Committee was of the view that this number may not be the correct estimate. Presently, the Indian Medical Register also contains the names of registered medical practitioners who are dead or retired from active practice. This hinders healthcare human resource planning. Therefore, the Committee recommended that the register should be maintained as a live database to provide a realistic assessment of number of practitioners.
Corruption: The Committee observed issues related to corruption in the MCI. Further, it noted that autonomy should be balanced with accountability. As MCI is funded by the government, therefore it should enforce accountability on the MCI. The Ministry should take measures to amend the present statute or enact a new legislation which allows the government to intervene in matters of corruption
On a concluding note, at the risk of sounding redundant; the NEET exam is the first step in the huge structural changes envisaged. No one is holier than others; in fact, the be it Government colleges or Private; there is an issue everywhere. The need of the hour is taming this mammoth corrupt system via structural changes. If the Modi Government is able to implement recommendations of PSC with the same vigor as the NEET exam issue, it would lead to huge prosperity for the generations to come.
ANNEXURE & NOTES:
RISE OF PRIVATE MEDICAL COLLEGES
India has seen the fastest growth in medical education sector in the world. In 1950 there were 28 colleges which reached a total of 384 colleges in 2014 with a total intake capacity of ~50,000 students.
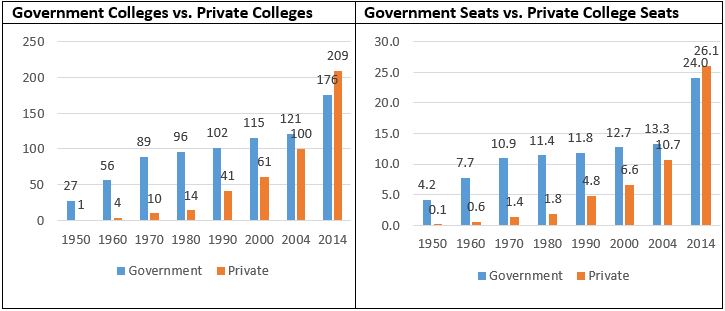
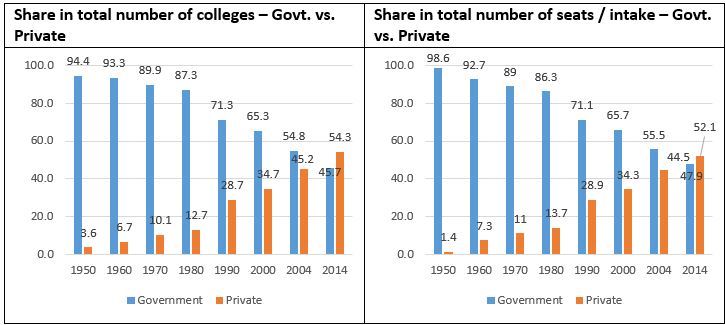
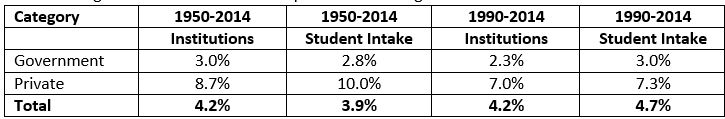
The tables and charts points to sharp increase in the number of private colleges vs., the government colleges. In fact, post liberalization, the government share in private seats has gone down significantly from 71.1% to 47.9. In fact, during the post liberalization era (as pointed from the table above), the average annual growth in the government institutions has lagged the overall growth rate from 1950.
Sources / Reference
http://www.academics-india.com/Parl_Panel_report_on_MCI.pdf
http://nihfw.org/pdf/Health.pdf
http://indiatoday.intoday.in/education/story/net-president-signs-ordinance-meical-exam/1/675828.html
http://www.thehindu.com/opinion/lead/doctors-by-merit-not-privilege/article4850500.ece
Reports:
- Parliamentary Standing Committee (PSC) on Health and Family Welfare’s Ninety Second Report on the Committee and Functioning of the Medical Council Of India dated 8th Mar 2016
- “Medical PG seats being sold! The Conundrum of Privatized Medical Education” , Indian J Med Res 135, February 2012, pp 255-257
- PRIVATE PLAYERS IN MEDICAL EDUCATION IN INDIA, by Satyajit Pattnaik, Dhananjay Sharma, ref., www.njcmindia.org
“Role of Private Sector in Medical Education and Human Resource Development for Health in India”; by Pradeep Kumar Choudhary, dated Oct 2014 published by “Institute for Studies in Industrial Development